Combating Digital Vision Syndrome
Digital Vision Syndrome has been a popular topic in the last few years as more of our time is dedicated to viewing our many digital devices. After long periods of use, many individuals, including myself, experience discomfort and visual problems.
What kind of symptoms are we talking about? Eyestrain, headaches, and dry eyes to name a few of the major offenders. The causes of Digital Vision Syndrome, however, are a little more difficult to pinpoint. It is typically a combination of various factors such as: poor lighting, posture, blue light emitted, uncorrected visual problems.
We take several steps to combat Digital Vision syndrome. Our first line of defense focuses on how we view our devices. Basic ergonomics such as positioning yourself at a computer screen so that the screen is 20 to 28 inches away from your eyes and between 15 to 20 degrees below eye level. Additionally, proper room lighting is imperative. Also make sure to take breaks by spending at least 20 seconds to look at something 20 feet away every 20 minutes of computer use. This is called the 20-20-20 rule.
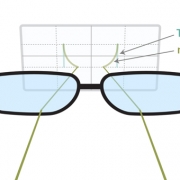
The second line of defense focuses on blocking the harmful blue light emitted from these devices. Research has shown that certain blue light has been linked to sleep issues and has a possible link to certain eye diseases. Special lens coatings can be added to your glasses to reduce this light.
The third line of defense focuses on reducing the amount of eyestrain by reducing the amount of focusing work your eyes do when looking something near and the amount of tension on the eye muscles. The newest technology in this category has been the Neurolens® released by eyeBrain Medical. Using the Neurolens Measurement Device, eye alignment is accurately measured for all distances. Any eye misalignment can cause the visual system to work harder which can lead individuals to experience the symptoms of Digital Vision Syndrome. The Neurolens® is a special lens design that corrects eye misalignment. By reducing the demand on the visual system symptoms of Digital Vision Syndrome can be greatly reduced or eliminated.
Blog contribution by Jonathan Kiriboon, Optometry Intern, College of Optometry, Western University of Health Sciences.
Sources: